Table of Contents
While more than 90 different types of sleep disorders could potentially be responsible for affecting people’s sleep, insomnia continues to be the most prevalent. Today, we’ll discuss what causes insomnia and a few treatment tips.
Deep sleep has become a prized commodity. The CDC recommends at least 7 to 9 hours of sleep every 24 hours for most adults. Work, school, parenting, and everyday errands make meeting that sleep quota difficult for most people.
While many people struggle to get enough sleep due to busy schedules, others are affected by sleep disorders. Statistically, estimates suggest that 50 to 70 million people in the United States suffer from a “disorder of sleep and wakefulness.”
Insomnia afflicts over 30% of the 70 million American adults with a sleeping disorder.

Insomnia is a prevalent sleep disorder affecting 35% of U.S. adults.
Insomnia
Insomnia Definition
Insomnia is a sleep disorder characterized by an individual’s inability to sleep and stay asleep throughout the night. It also includes waking up too early and being unable to fall back asleep. Insomnia results in non-restorative sleep that affects the person’s mood, mental well-being, and ability to function normally throughout the day.
Persistent, chronic insomnia can often lead to physical health problems over time. For example, it increases the risk of certain conditions, including blood pressure, diabetes, coronary heart disease, and cancer.
Common symptoms of insomnia include:
- Difficulty in falling asleep
- Waking up in the middle of the night or too early in the morning
- Feeling fatigued even after a night’s sleep
- Daytime tiredness (40% of people with a sleeping disorder report falling asleep accidentally during the day, while 5% report falling asleep while operating a vehicle.)
- Inability to focus
- Memory problems
- Frequent errors or accidents
- Lack of motivation
- Lack of energy or lethargy
- Mood disturbances
Insomnia can impact other aspects of your life, including your performance at work and school, cognitive functionality, concentration, decision-making skills, etc. A 2011 study showed that in the U.S., 63 billion dollars are lost in the workplace because of lowered workplace performance due to insomnia. The effects of insomnia may even have repercussions on your relationships.
Prevalence
Approximately 30% to 35% of adults in the United States experience brief insomnia symptoms. The American Psychiatry Association or APA states that one out of three American adults reports insomnia symptoms. About 6% to 10% experience symptoms at a severity that can lead to an official diagnosis of insomnia.
Another study reports that at least 25% of people in the U.S. experience acute insomnia every year. While 75% of those with acute insomnia recover, over 21% remain poor sleepers, and 6% develop chronic insomnia.
Types
The stats mentioned above bring to light the realization that insomnia is not ubiquitous. While some people deal with it infrequently and for short periods, others have a more persistent or chronic type of insomnia.
The types of insomnia are classified based on duration, cause, and severity.
- acute insomnia is transient and lasts for a short time, such as 1 day to 2 weeks.
- Chronic insomnia can last for months or even years. Chronic insomnia occurs when a person cannot sleep or has difficulty sleeping for three or more days a week over three months. According to the American Sleep Association (APA), around 30% of people with a sleeping disorder have short-term insomnia, while 10% have chronic or long-lasting insomnia.
- Onset insomnia is the difficulty of initially falling asleep. This type of insomnia may be acute or chronic.
Based on causes
- primary insomnia is the issue of sleeplessness, while secondary insomnia results from another underlying disorder or health issue.
Based on severity
- Mild insomnia can be characterized as a lack of sleep that results in tiredness.
- Moderate insomnia affects daily functioning and well-being.
- Severe insomnia can disrupt cognitive function, negatively affecting the person’s quality of life.
Risk Factors for Insomnia
Before we discuss the causes of insomnia, it’s essential to address the risk factors that increase the likelihood of developing it.
Age & Gender
Insomnia can occur regardless of age, as 30% of children with poor sleeping habits develop behavioral insomnia—however, your chances of experiencing insomnia increase as you grow older.
Regarding gender, women are more likely to develop insomnia than men. Often, discomfort due to hormonal changes during menstruation, pregnancy, and menopause can lead to insomnia.
The National Heart, Lung, and Blood Institute (NHLBI) considers lower income, a sedentary lifestyle, disturbed sleep cycles, emotional disorders, and stress as risk factors for developing insomnia.
Sleep Cycle Disruption
Adjustment insomnia affects around 20% of people annually due to long work hours, night shifts, noise or light disturbing the sleep-wake cycle, traveling through different time zones (jet lag), or uncomfortable temperatures.
Lifestyle
Lack of physical activity prevents your body from getting tired enough to fall asleep easily. Lifestyle habits such as drug and alcohol use, smoking, caffeine consumption, watching T.V., using electronic devices at night, and napping during the day are what causes insomnia, among other things.
Stress, Anxiety, and Other Mental Health Problems
APA reports that 3% of the population with insomnia experiences it due to mental health conditions such as stress, anxiety, drug withdrawals, substance abuse, or prescription abuse. Psycho-physiological insomnia affects 2% of the population, especially people with anxiety and stress caused by work, relationships, friendships, etc.
What Causes Insomnia?
A study is discussing the prevalence, etiology, and consequences of insomnia states hyper-arousal stimulated by activities, circumstances, and other risk factors as causes of insomnia. The state of hyper-arousal can be mental, physical, or both.
Hyper-arousal may further trigger or worsen other mental and physical health conditions. Let’s take a closer look at some of the leading causes of insomnia.
Mental Health Disorders
Mental health disorders are often accompanied by insomnia or sleep-related issues. For instance, 80% of people with depression experience daytime sleepiness and insomnia. Another statistic in the MSD Manual suggests that 40% of people with chronic insomnia also have a mental health disorder.
Associated mental health disorders include major depression, anxiety, and bipolar disorder.
In some cases, insomnia is caused by mental health disorders. Insomnia can also worsen mental health issues. Insomnia and mental health issues can turn into a vicious cycle, with one feeding the other.
Such disorders lead to pervasive negative thoughts that cause negative mental hyper-arousal, which may keep you up at night for hours. Hyperarousal disturbs sleep and can cause insomnia (on-set or maintenance).
Stress
According to the American Psychological Association’s Stress in America ™ 2020 report, two out of three people experienced some form of stress throughout 2020 due to COVID-19, meaning that 60% of the American population experienced psychological stress due to pandemic-related uncertainty.
Stress is prevalent among the American population, whether caused by a traumatic or economic situation.
Psychological stress often leads to interrupted sleep cycles. As the body experiences stress, hyper-arousal prevents you from sleeping. The cause of insomnia may be attributed to psychological stress. If left unaddressed, stress-induced insomnia causes further stress, which creates even more sleep issues. In short, stress can lead to an unbreakable insomnia-sleep cycle where you wake up at the same time in the middle of the night, unable to fall back asleep.
Physical Health Issues
In addition to mental health disorders and illnesses, physical health concerns such as chronic pain can disturb sleep cycles and cause insomnia. Pain not only makes it difficult to lie comfortably in bed, but it also causes psychological stress. Physical pain, added to psychological stress, results in disrupted sleep-wake cycles.
Physical illnesses include diabetes, pain caused by peripheral neuropathy (damage in the nerves outside of the brain and spinal cord), blood sugar irregularities, frequent urination, respiratory problems, and nervous system conditions. All of these ailments can be contributing factors to the development of insomnia.
Neurological diseases that cause insomnia
Neurodegenerative diseases may be the cause of insomnia.
Conditions such as dementia, Alzheimer’s, and attention deficit hyperactivity disorder (ADHD) can disrupt circadian rhythms. These conditions can worsen sleep quality and can lead to the development of insomnia. Children with autism spectrum disorder may also develop sleeping disorders, which can persist into adulthood.
Medication
In some cases, medication might be the reason you experience insomnia and other sleeping disorders. Medication for blood pressure, asthma, and depression can cause sleep problems. Furthermore, when medication is stopped, withdrawal symptoms can cause reactions in the body that may prevent you from falling asleep.
Sleep Disorders
Obstructive sleep apnea (OSA), characterized by pauses in breath and temporary sleep interruptions, can cause insomnia. Research suggests that over 22 million Americans are affected by OSA, which can cause sleep disorders.
Other sleep-related problems, such as restless leg syndrome and parasomnias, such as sleep paralysis and sleepwalking, can also cause insomnia.
Irregular Sleep Schedules affecting insomnia
Irregular sleep schedules disrupt your body’s natural circadian rhythm. The circadian rhythm is a sleep-wake cycle that is adjusted to daylight and the darkness of night. When the sun rises, your body’s circadian rhythm directs the brain to wake up. When the sun goes down, it tells it to become sleepy.
Jet lag, working the night shift, or simply staying awake past bedtime can disturb your circadian rhythm. Jet lag increases acute insomnia.
Lifestyle Choices
Using electronic devices late at night, working overtime, playing video games, taking naps during the day, and sleeping in might throw off your sleep schedule and disrupt your circadian rhythm.
Diet also has a significant impact on your sleep. Caffeine, nicotine, and alcohol are the obvious culprits for acute insomnia. Heavy or spicy meals at night can cause digestive distress, leading to insomnia and daytime sleepiness.
Insomnia during Pregnancy
During pregnancy, anatomical, hormonal, and physiological changes can affect sleeping patterns. For example, an enlarged abdomen, sore breasts, swollen ankles, and increased pressure on the lower back can cause discomfort while lying down.
Nausea, disturbed breathing, pressure on internal organs, increased need to urinate (nocturia), sciatica, acid reflux, restless leg syndrome, etc., can cause insomnia during pregnancy.
Insomnia & Childhood
Insomnia is a growing problem among children and teenagers. A study estimated that up to 23.8% of teenagers experience insomnia. Natural biological changes, staying up late to study, playing video games, or using social media are to blame for insomnia among teenagers.
Overscheduling, school and work-related stress, excessive caffeine intake, drug use, anxiety, depression, and busy social life can contribute to teenage insomnia.
Dealing with Insomnia
If you are experiencing insomnia, you must take the necessary measures to improve your sleeping habits. Learn some relaxation techniques and integrate them into your routine as a remedy for insomnia.
Consult a physician or sleep expert if the problem persists. Neglecting to do so may cause significant disruptions that negatively impact your health and lower your quality of life.
Counselling, cognitive-behavioral therapy (CBT), prescription medication, melatonin, and sleep aids (over-the-counter) are some treatments for insomnia.
Despite treatments being available, you’re better off taking preventative measures. As the Dutch philosopher, Desiderius Erasmus wrote, “prevention is better than cure.”
Making the following changes can help prevent insomnia:
- Going to bed early
- Associating your bedroom only with sleep
- Avoiding the use of electronic devices before bed
- Blocking light in the room
- Establishing an evening routine
Switching to a healthy diet, non-smoking, reducing caffeine and alcohol intake, and engaging in relaxation techniques can dramatically improve your sleep.
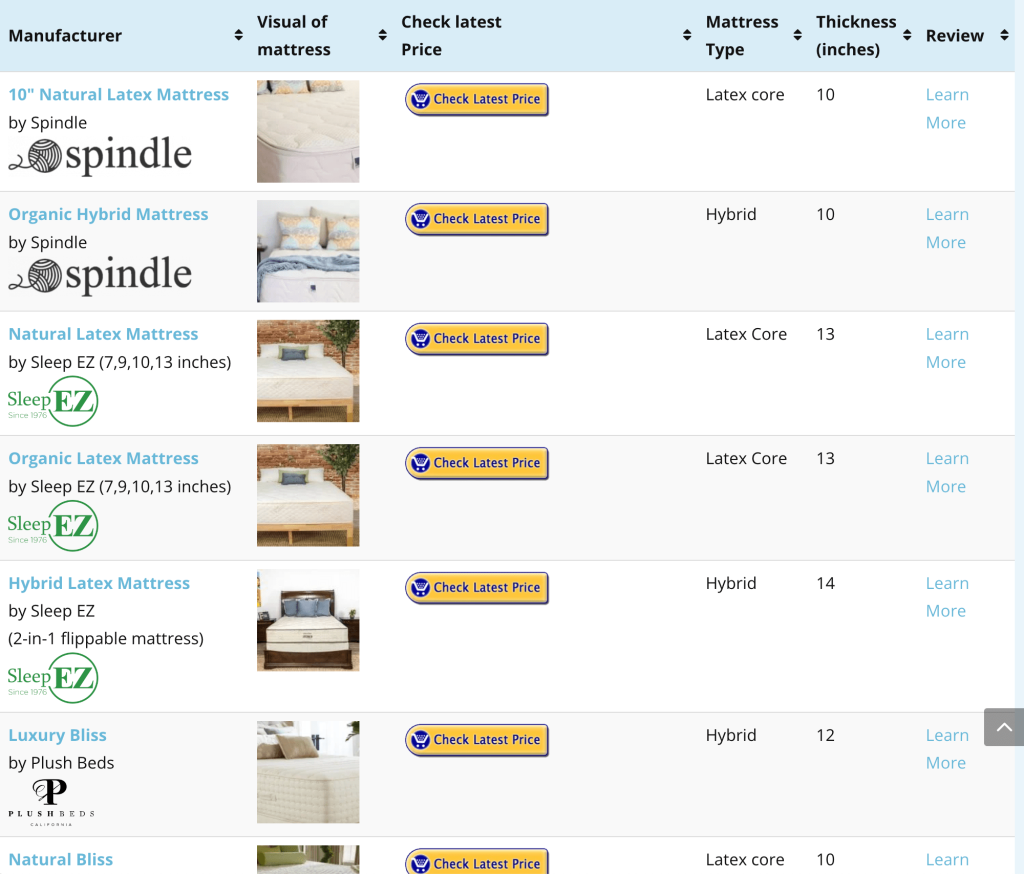
Your mattress could very well be why you can’t sleep. If you’re dealing with acute insomnia, switching to a natural latex mattress may be a solution. Natural latex mattresses have many benefits that allow you to sleep in comfort. These include:
- Contouring to fit your body shape;
- Natural latex is breathable, preventing excessive sweating during the night;
- Improved motion isolation so you don’t wake your partner
- Reinforced edges thanks to a pocketed coil layer
- No off-gassing as natural latex foam is free of VOCs (volatile organic compounds)
Whether it’s an all-latex natural mattress or a hybrid natural latex mattress (latex foam + spring coils) you prefer, there are plenty of options for natural latex mattresses. To find a solution befitting your sleeping needs and sleeping position, go to https://www.naturalmattressfinder.com/latex-mattresses/
References
- Institute of Medicine (U.S.) Committee on Sleep Medicine and Research; Colten HR, Altevogt BM, editors. Sleep Disorders and Sleep Deprivation: An Umber Public Health Problem.Washington (D.C.): National Academies Press (U.S.); 2006. https://www.ncbi.nlm.nih.gov/books/NBK19961/#a2000f7efrrr00394
- NHLBI (National Heart, Lung, and Blood Institute). National Sleep Disorders Research Plan, 2003. Bethesda, MD: National Institutes of Health; 2003.
- Kessler, R. C., Berglund, P. A., Coulouvrat, C., Hajak, G., Roth, T., Shahly, V., Shillington, A. C., Stephenson, J. J., & Walsh, J. K. (2011). Insomnia and the performance of U.S. workers: results from the America insomnia survey. Sleep, 34(9), 1161–1171. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3157657/
- Sateia MJ. International classification of sleep disorders-third edition: highlights and modifications. Chest. 2014 Nov;146(5):1387-1394. https://pubmed.ncbi.nlm.nih.gov/25367475/
- https://www.psychiatry.org/patients-families/sleep-disorders/what-are-sleep-disorders
- University of Pennsylvania School of Medicine. One in four Americans develops insomnia each year: 75 percent of those with insomnia recover. (2018) https://www.sciencedaily.com/releases/2018/06/180605154114.htm
- The Centers for Disease Control and Prevention. Sleep and Sleep Disorders: How Much Sleep Do I Need? https://www.cdc.gov/sleep/about_sleep/how_much_sleep.html
- Buysse D. J. (2013). Insomnia. JAMA, 309(7), 706–716. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3632369/
- The American Sleep Association. Sleep and Sleep Disorder Statistics. https://www.sleepassociation.org/about-sleep/sleep-statistics/
- NHLBI (National Heart, Lung, and Blood Institute). Insomnia. https://www.nhlbi.nih.gov/health-topics/insomnia
- Roth T. Insomnia: definition, prevalence, etiology, and consequences. J Clin Sleep Med. 2007 Aug 15;3(5 Suppl): S7-10. https://pubmed.ncbi.nlm.nih.gov/17824495/
- Neckelmann D, Mykletun A, Dahl AA. Chronic insomnia as a risk factor for developing anxiety and depression. Sleep. 2007 Jul;30(7):873-80. https://pubmed.ncbi.nlm.nih.gov/17682658/
- The American Psychological Association. Stress in America™ 2020: A National Mental Health Crisis. 2020. https://www.apa.org/news/press/releases/stress/2020/report-october#:~:text=The%202020%20Stress%20in%20America,shape%20a%20brighter%20future%20together.
- Kalmbach DA, Cuamatzi-Castelan AS, Tonnu CV, Tran KM, Anderson JR, Roth T, Drake CL. Hyperarousal and sleep reactivity in insomnia: current insights. Nat Sci Sleep. 2018 Jul 17;10:193-201. https://pubmed.ncbi.nlm.nih.gov/30046255/
- Finan PH, Goodin BR, Smith MT. The association of sleep and pain: an update and a path forward. J Pain. 2013 Dec; 14 (12):1539-52. https://pubmed.ncbi.nlm.nih.gov/24290442/
- Medline Plus. Degenerative Nerve diseases. https://medlineplus.gov/degenerativenervediseases.html
- Franklin KA, Lindberg E. Obstructive sleep apnea is a common disorder in the population-a review on the epidemiology of sleep apnea. J Thorac Dis. 2015 Aug;7(8):1311-22. https://pubmed.ncbi.nlm.nih.gov/26380759/
- Silvestri R, Aricò I. Sleep disorders in pregnancy. Sleep Sci. 2019 Jul-Sep;12(3):232-239. https://pubmed.ncbi.nlm.nih.gov/31890101/
- Donskoy I, Loghmanee D. Insomnia in Adolescence. Med Sci (Basel). 2018 Sep 1;6(3):72. https://pubmed.ncbi.nlm.nih.gov/30200388/