Table of Contents
Narcolepsy causes a disruption in the normal function of your biological clock. Due to poor regulation of the sleep-wake cycle caused by a chemical imbalance in the brain, patients may find it difficult to stay awake during the day. Scientists refer to this as excessive daytime sleepiness or EDS.
Generally speaking, normal sleep consists of several stages that are numbered from 1 to 4. The most important stage of sleep is the rapid eye movement (REM) stage, where your eyes move from one side to the other. The REM stage occurs 90 minutes after falling asleep; however, patients with narcolepsy often go through this stage within minutes after falling asleep.
According to reports, narcolepsy affects between 20–67 people out of 100,000 in the United States. This prevalence is relatively low compared to other sleep disorders, such as insomnia.
However, some experts believe that the prevalence of narcolepsy is much higher than the declared numbers due to the underdiagnosis of this condition. You see, many patients experience the symptoms of narcolepsy for years before consulting with a sleep doctor and getting a diagnosis. As a result, the prevalence of narcolepsy could be as high as 180 people out of 100,000.
The scientific community categorizes narcolepsy into two types (more on that later). The first type – narcolepsy type 1 – is 2 to 3 times more common than narcolepsy type 2.
In this article, we will discuss everything you need to know about this condition, including narcolepsy types, narcolepsy causes, narcolepsy symptoms and narcolepsy diagnosis & treatment options.
The types of narcolepsy
The international classification of sleep disorders 3 (ICSD-3) categorizes narcolepsy into two types:
Narcolepsy Type 1 (NT1)
In this type of narcolepsy, patients present with cataplexy, which refers to the sudden loss of muscle tone. In other words, a person may be standing then suddenly falls to the ground after losing the tonicity of his/her muscles.
Note that some patients with NT1 may not experience cataplexy. Having low levels of hypocretin-1 is enough to confirm the diagnosis.
Unfortunately, cataplexy occurs in the vast majority of patients with low levels of hypocretin-1, regardless of previous medical history.
Narcolepsy Type 2 (NT2)
Unlike NT1, narcolepsy type 2 does not present itself with cataplexy or low levels of hypocretin-1s.
If you have been diagnosed with NT2 but you experience cataplexy or your levels of hypocretin-1 drop at some point, your doctor may reclassify your diagnosis.
According to reports, this reclassification occurs in 10% of cases.

Daytime sleepiness is one of the most prominent symptoms of narcolepsy.
Narcolepsy causes
The causes of narcolepsy are multifactorial with many vague points. However, researchers managed to get some insight into the biochemistry of NT1 and NT2. We should note that scientists know more about NT1 than NT2.
Unfortunately, the lack of a comprehensive understanding of narcolepsy made it challenging to prevent or cure this condition.
With that said, here is what we know about the triggers of NT1 and NT2:
NT1
The primary defect with NT1 is the necrosis (i.e., cellular death) of the neurons responsible for the secretion of hypocretin (i.e., orexin). This chemical regulates the sleep-wake cycle. According to one study, patients with NT1 lose more than 90% of their hypocretin-producing neurons.
The hypothesis to explain this disease boils down to two components:
The nature part – this refers to being genetically predisposed to developing narcolepsy. If you have a family member with this condition, your risk will inadvertently increase. A family history of NT1 increases your risk by 1–2%.
According to research, 98% of people with NT1 have a gene variant known as DQB1*060215. The phenotypic expression of this gene produces proteins that control some aspects of the immune response. Therefore, researchers believe that it might be responsible for an autoimmune response against your neurons.
The nurture part – as opposed to the nature part, environmental factors can also contribute to NT1. Experts believe that an external trigger interferes with the normal function of your immune system, which leads to the destruction of hypocretin-secreting neurons. The most common culprit is a viral infection, such as H1N1. However, researchers found that several types of viral infections could be responsible for triggering NT1.
While the two components of this hypothesis may explain the triggering of NT1, there seem to be several factors that contribute to this disease. Differently put, NT1 causes are multifactorial, but the final result always leads to the destruction of neurons and low levels of hypocretin-1.
Secondary narcolepsy is also possible when another disease leads to the destruction of hypocretin-secreting neurons. However, the incidence of this subtype is extremely rare.
NT2
While scientists know a fair share about the pathophysiology of NT1, they still have a long way to go with NT2.
The most commonly believed theory to explain this condition states that NT2 is a less severe form of NT1. In other words, the loss of hypocretin is not extensive to cause cataplexy. Another theory suggests that NT2 is the precursor of N1. However, only 10% of patients with NT2 develop NT1.
When patients present with NT1, reporting a viral infection in the medical history is more likely than with NT2.
In summary, scientists are still investigating the causes of NT2 with little progress.

Narcolepsy can cause excessive daytime sleepiness when studying or at work.
The signs and symptoms of narcolepsy
The signs and symptoms of narcolepsy can severely impact the patient’s quality of life.
Here are the most common symptoms:
Excessive daytime sleepiness (EDS)
EDS is the cardinal symptom of narcolepsy since it affects all people with this condition. EDS is defined as the the irresistible urge to sleep, which generally occurs in monotonous situations (e.g., working on your desk, sitting on a chair, standing without movement).
In some cases, the severe drowsiness leads to lapses in attention, where patients are unable to focus during a lecture or presentation. Additionally, falling asleep without warning is not uncommon.
Once the narcoleptic patient takes a nap, he/she will feel temporarily refreshed.
Automatic behaviours
After experiencing EDS for a while, people tend to develop these repetitive patterns and behaviours to cope with sleepiness.
An example of this includes an employee who starts drawing lines on a paper during a meeting to avoid creating a monotonous environment.
Disrupted nighttime sleep
Narcolepsy causes disrupted nighttime sleep is a very common symptom in patients.
During these episodes, patients wake up multiple times during the night without any stimuli. Besides sleep fragmentation, sleep apnea is also more prevalent in patients with narcolepsy relative to the general population.
Sleep paralysis
People with narcolepsy are at a higher risk of developing sleep paralysis, which describes a feeling of complete immobility prior to falling asleep or just after waking up.
Sleep paralysis is part of a set of disorders known as parasomnias.
Learn more about parasomnias by clicking on this link (insert link of the previous article).
Sleep-related hallucinations
Narcolepsy causes hypnagogic hallucinations (imagery that occurs while falling asleep) or hypnopompic hallucinations (imagery that occurs after waking up) in certain patients.
These hallucinations are particularly frightening for patients and can negatively impact their quality of life.
Cataplexy
Cataplexy describes the sudden loss of muscle tonicity. As we mentioned above, cataplexy only occurs in patients with NT1.
Interestingly, cataplexy often occurs in response to positive emotions (e.g., laughter) and lasts for a few minutes. However, it may take many years for a narcoleptic patient to develop cataplexy.
The frequency of cataplexy episodes varies greatly from one patient to another. For instance, some people have a few episodes per year, whereas others experience several episodes in one day.
A final word about narcolepsy symptoms
While all narcoleptic patients have EDS, less than ¼ of them have the other symptoms we listed above. Furthermore, it is unlikely for one patient to experience all the symptoms of narcolepsy at once.
The diagnosis of narcolepsy
Due to the number of conditions that have similar symptoms to narcolepsy, it may be challenging to distinguish this disease from other sleep disorders. Therefore, a comprehensive analysis of the patient’s medical history, symptoms, physical exam findings, and test results becomes indispensable to confirm the diagnosis.
Furthermore, the relatively uncommon nature of narcolepsy causes its misdiagnosis in hundreds of cases (e.g., depression, anxiety, sleep apnea, hypersomnia).
Generally speaking, the efforts to diagnose narcolepsy begin with a review of the patient’s medical history to note the presence of concurrent sleep disorders or organic conditions that may explain their symptoms.
The next step revolves around deciphering their chief complaint. The following questions may help with this step:
- Why is the patient not sleeping?
- What made him/her visit the doctor today?
- Are the symptoms getting worse?
- Are there any factors that trigger EDS or cataplexy?
- Is the patient taking any pharmacological drugs?
- What are the sleeping habits and patterns of the patient?
When narcolepsy is suspected in a child, gathering information from a family member becomes crucial to add context to their symptoms.
Once the doctor completes the two steps, it is time for some additional tests.
Tests for narcolepsy
The primary purpose of these tests is to evaluate the sleep pattern and EDS of the patient. For instance, the Epworth Sleepiness Scale (ESS) assesses the patient’s symptoms subjectively. In other words, the test records what the patient is reporting about their state of sleepiness.
Another test is polysomnography (PSG), which involves sensors to monitor the activity of your brain and body. PSG requires a specialized clinic equipped with the necessary instruments. You will also need to spend at least one night at the clinic in order to evaluate your symptoms.
The day following the PSG test, an objective assessment known as the Multiple Sleep Latency Test (MSLT)may be conducted in order to aid in the diagnosis.
During this test, the doctor will ask the patient to fall asleep at 5 intervals. The patient will remain connected to the sensors of the PSG. The primary defect reported on this test is the rapid onset of sleep and the REM cycle in patients with narcolepsy.
The final test that may be helpful is getting a cerebrospinal fluid (CSF) sample to measure the levels of hypocretin. The doctor will perform a spinal tap (i.e., lumbar puncture) to draw the CSF.
If the patient has low levels of hypocretin, it may help in diagnosing narcolepsy and differentiating NT1 from NT2.
Diagnostic Criteria for Narcolepsy
Due to the complexity of diagnosing narcolepsy, experts developed standardized diagnostic criteria for sleep disorders. Consequently, the diagnosis of narcolepsy and other sleep disorders becomes more accurate, and the differentiation between NT1, NT2, and other forms of hypersomnia is more obvious.
The first criterion in a narcolepsy diagnosis is significant EDS (excessive daytime sleepiness) lasting in excess of 3 months. As we previously mentioned, patients with NT1 must have cataplexy or low levels of hypocretin in their cerebrospinal fluid. Additionally, the rapid onset of the REM cycle on the MSLT is part of the criteria.
As for NT2 (Narcolepsy Type 2), it shares similar results on the MSLT (multiple sleep latency test) with NT1(Narcolepsy Type 1); however, cataplexy and low levels of hypocretin are not present.
Unfortunately, many sleep disorders share similar symptoms to NT2, which makes the diagnosis quite challenging. For this reason, it is preferable to see a specialized sleep doctor who has a lot of experience with narcolepsy. Your doctor will start by eliminating other potential diagnoses through the analysis of your medical history, symptoms, and test results.
The treatment options of narcolepsy
Currently, there is no cure for narcolepsy; however, the goal of therapy is to control the symptoms, ensure patient safety, and improve quality of life.
For many people, narcolepsy remains a stable condition. Additionally, some symptoms improve after the age of 18. However, neuroscientists are still uncertain about why the disease presents itself differently in people.
Generally speaking, the treatment for both types of narcolepsy is similar; with that said, NT2 does not involve any medications for cataplexy.
Your doctor may suggest a combination of medical treatment and behavioural therapy to decrease the severity and frequency of symptoms. In some cases, EDS (excessive daytime sleepiness) remains problematic despite appropriate treatment.
All patients should get a tailored management plan from their doctor that takes into consideration every aspect of their health.
6 Behavioural Approaches to Treatment
Behavioural therapies involve certain habits that you can integrate into your daily life.
Here are some behavioural changes that could help patients with narcolepsy:
1. Planning short naps
Short naps are an excellent way to refresh your energy if you have narcolepsy. Practicing this habit will undoubtedly reduce EDS; however, be ready to make some adjustments at school or work.
2. Having healthy sleep hygiene
Improving your sleep hygiene is crucial to combat narcolepsy. You can start with the little things, such as setting a consistent sleep schedule, reducing distractions from light and noise while in bed, and limiting the use of digital devices before bed.
All of these practices can dramatically help you sleep better, which lowers the chances of EDS during the morning.
3. Avoiding alcohol and other sedatives (e.g., Xanax)
The intake of any sedative substance can induce sleepiness during the day, which is the last thing you’d want as someone with narcolepsy.
Instead, try to exercise after waking up to prevent early EDS and keep going through the day.
4. Driving with caution
Narcoleptic patients should be extra careful when it comes to driving. In fact, you should talk with your doctor about safe driving since EDS is a common symptom during long rides that involve a monotonous pattern.
5. Eating a balanced diet
If you are diagnosed with narcolepsy, your risk of obesity increases. Therefore, you need to maintain a healthy diet and avoid sugar-rich foods and unhealthy fats.
Talk with your doctor or nutritionist to come up with a dietary plan that meets your needs.
6. Exercising
Exercising regularly helps improve the quality of your sleep and prevents obesity. For best results, try mixing cardio sessions with strength training exercises.
7. Seeking support
Support groups and mental health professionals can aid narcolepsy sufferers with emotional distress and prevent psychiatric disorders, such as depression, anxiety, and social withdrawal.
Is your mattress optimized for the best sleep?

The Cedar Natural Luxe has an organic cotton cover, a wool fire barrier, 100% natural Dunlop latex, Alpaca wool, and a spring coil unit to keep you well supported.
If your mattress is sagging, lumpy, too hard or too soft, it might be a good idea to replace it. Furthermore, most conventional mattresses off-gas VOCs into your home environment. VOCs are time-released from components like polyester fibre and fabric, polyurethane foam (memory foam, gel foam, cooling gel foam) and polyester fibre.
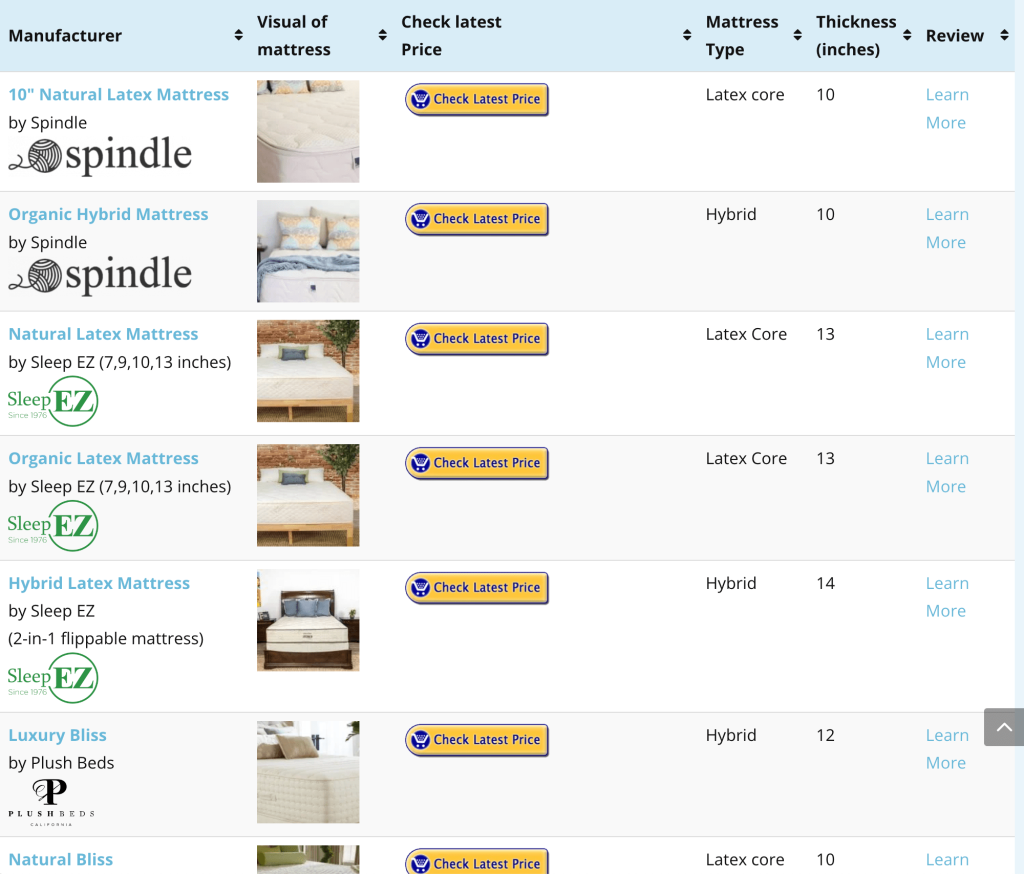
A durable alternative to a sagging and toxic polyurethane mattress is a natural latex mattress. Natural latex mattresses offer a buoyant and supportive sensation and last at least 3X longer than polyurethane mattresses. Find the most optimal thickness and firmness by consulting our natural latex mattress interactive comparison table.
Medications
Regardless of the benefits of behavioural therapies, most patients still need to receive pharmacological drugs to address the symptoms of narcolepsy.
Like all drugs, narcolepsy medications can cause side effects, which vary in frequency and severity from one individual to another. In order to treat your condition successfully, compliance with the doctor’s or pharmacist’s instructions is fundamental.
The following list will cover the most common medication that is used to treat narcolepsy:
Modafinil and armodafinil
These two drugs are typically the first-line treatment for EDS. They both have a similar chemical structure and work in a similar way.
Methylphenidate
This is a type of amphetamine, which is a stimulant drug that can reduce EDS.
Solriamfetol
Solriamfetol was approved by the FDA in 2019. It has shown substantial benefits for EDS sufferers. Solriamfetol helps patients who cannot take modafinil.
Sodium Oxybate
Sodium Oxybate controls cataplexic attacks, EDS, and nighttime sleep disturbances. However, the onset of this medication is long (may take months before it’s effective).
Pitolisant
Similar to Solriamfetol, this drug was FDA approved in 2019. It is a wakefulness-promoting drug that positively impacts cataplexy.
Clearly, narcolepsy medication will have varying effects from one person to another. Additionally, some patients may experience certain side effects, which is why you need to work with your doctor to find the most beneficial medication and dosage.
Let your doctor or pharmacist know if you experience any side effects, especially if you are taking other treatments. There may be a risk of interactions between medications.
Narcolepsy Treatment and Children
Treatment for children with narcolepsy is somewhat similar to adult treatment; however, the choice of medication and dosage may be slightly different.
For instance, children need a cardiovascular assessment before the prescription of stimulant drugs. This recommendation comes straight from the American Academy of Pediatrics.
Narcolepsy Treatment and Pregnancy
There is limited data about the safety of narcolepsy drugs for pregnant and breastfeeding women. Doctors recommend the interruption of narcolepsy medication when you are trying to conceive or during the process of pregnancy/breastfeeding, according to one survey.
The discontinuation of treatment may necessitate some behavioural changes and accommodations to cope with the symptoms of narcolepsy. For instance, you may want to take a break from work during the day to nap.
The prognosis of narcolepsy
Following the proper management and treatment plans for narcolepsy can considerably improve a patient’s quality of life on personal and professional levels. Conversely, untreated narcolepsy could have detrimental psychological and social consequences.
For instance, children with narcolepsy often have difficulty with school exams, social interactions, and making friends.
On the other hand, adults commonly perceive the symptoms of narcolepsy as embarrassing, which may lead to social isolation. Additionally, sufferers of narcolepsy report issues with relationships, sexual activity, and professional life. Note that the side effects of narcolepsy treatments may be responsible for some of these issues.
Sleep attacks due to EDS may lead to memory problems, interpersonal problems, lack of focus while at work, and personality changes. In fact, many employers and coworkers perceive the symptoms of narcolepsy as a sign of laziness, demotivation, and inattentiveness.
According to one study, 24% of patients with narcolepsy had to quit their job and 18% got fired due to the symptoms of this disease.
Unfortunately, people often mistake narcoleptic patients for illicit drug users. For this reason, patients are advised to inform their employers about their conditions to explain any unwanted symptoms in the workplace.
Another reason you would want to inform your boss about narcolepsy is due to the medication you may need to take. Certain drugs that treat narcolepsy may give a positive result on a screening test for amphetamines, which is commonly conducted during the pre-employment process.
A final word about Narcolepsy
Narcolepsy causes an interference with the normal functioning of one’s biological clock. When the sleep-wake cycle is disrupted, patients experience a variety of symptoms that negatively impact their health and quality of life.
Dealing with narcolepsy is a difficult task that requires the cooperation of the sufferer and his/her doctor.