Table of Contents
You have most likely experienced removing the covers on a warm night at one point in your life. Or, you may have woken up soaked from head to toe in sweat after a particularly intense nightmare. While bothersome, sweating during the night is generally not a problem. But suppose you regularly wake up in soaked bed sheets and drenched pajamas. In that case, you could be experiencing a medical condition known as sleep hyperhidrosis, or night sweats, according to the Mayo Clinic. The causes of sweating at night in men may be due to environmental, physiological, and medication.
Sleep is a vital function that allows your mind and body to regenerate, leaving you revitalized and alert when you wake up. A lack of sleep, however, can make you more irritable, scatter-brained, and less able to excel in daily life. For many men, night sweats represent a prevalent barrier to high-quality sleep.
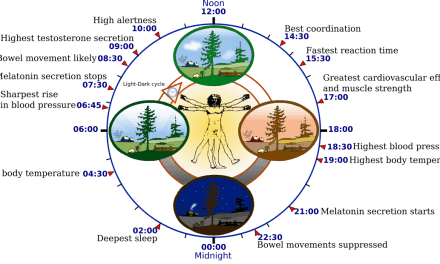
Regulation of sweating is complex, involving both thermoregulatory and non-thermoregulatory mechanisms in the brain and body. Generally, our bodies prefer to stay at approximately the same temperature or “thermoneutral zone.” The thermoneutral zone fluctuates on a circadian rhythm, and your body usually cools throughout the night. Your lowest temperature and sweat threshold occurs a few hours before you naturally wake up. Therefore, thermoregulatory defenses such as sweating are stimulated when threshold levels in core body temperature are reached. When the body is at a lower temperature, it shivers in response, thus raising the temperature. When the body is overheated, the thermoneutral zone rises above average, resulting in sweating as the body releases heat for cooling.
Now, it’s important to distinguish night sweats from occasionally being sweaty at night, usually for an environmental reason. You may awaken after sweating if you have too many blankets or your bedroom is too warm. These episodes should not be labeled as ‘night sweats’ and do not represent a medical problem. At the same time, there is no universal definition for night sweats. In general, they are defined as recurrent episodes of excessive sweating during the night that requires: no changing of clothes (mild), sleep disturbed by the need to wake up to wash face or body areas, but no clothing change required (moderate), or requiring changing of bedclothes and bedding (severe).
Night sweats are relatively common, affecting both men and women. Although harmless, excessive sweating can negatively impact sleep quality and signify a severe underlying condition or disease. 10 to 40 percent of adults experience night sweats for a certain period during the year.
Several factors can interfere with men’s temperature-balancing system, including physical, medical, and psychological factors. A hot shower, a hot beverage, or exercising shortly before bed can trigger night sweats. However, night sweats can involve complex medical conditions, and consultation with a physician, therapist, or sleep specialist may be necessary.
Below are several causes of night sweats in men.
Anxiety
Many people sweat when they get nervous or stressed. Anxiety activates the body’s stress response, increasing perspiration. The purpose of the stress response is to mobilize the body with a surge of energy. It does so by activating your sympathetic nervous system, or SNS.
When stress grows out of control, your SNS becomes aroused, driving adrenaline and triggering cortisol and other stress hormones. Your sweat glands are then activated by nerves which can be sensitive to these changes in emotions and hormones.
During activation of the stress response, your heart begins to beat faster, and your breathing quickens. Your body is preparing to expend energy. This shift increases your body temperature.
When dealing with anxiety, you are likely to experience other physical symptoms alongside sweating, such as:
- Dizziness
- Shortness of breath
- Aches and pains
- Restlessness and lack of concentration
Sleep Apnea
One of the most common signs of this sleep disorder is night sweats.
A study in 2013 found that 30 percent of men in the general population with OSA (obstructive sleep apnea) reported night sweats.
Sleep apnea happens when breathing is disrupted while you sleep. The tongue and throat muscles relax and block the airways (obstructive sleep apnea, or OSA), making exhaling air difficult. It affects about 25% of American men, ages 30 to 70, and tends to occur more in people over 50 who are overweight. OSA is 3-5 times more likely to occur in men than women due to the anatomical differences in airway shape and size. When left untreated, the condition may stop your breathing several times per night.
Aside from night sweats, sleep apnea may have the following symptoms:
- Daytime sleepiness
- Snoring
- Dry mouth or a sore throat in the morning
If you suspect you have sleep apnea, visit a sleep specialist for a diagnosis.
Treatment may include lifestyle changes like losing weight, exercising, and avoiding alcohol.
Hyperhidrosis
Hyperhidrosis is a medical term used to describe a situation where nerves that regulate your sweat glands become hyperactive. This condition may cause excessive sweating even when no triggers, such as temperature or physical activity, are present. The sweating may be enough to soak through clothing and can even result in skin issues due to its constant exposure to moisture.
Hyperhidrosis is very common, affecting about 15 million Americans, with the primary symptom being excessive sweating, which can occur during the day and at night.
Some people develop primary hyperhidrosis, which refers to hyperhidrosis not elicited by underlying health issues. However, underlying conditions such as diabetes and infections may also cause hyperhidrosis, which is referred to as secondary hyperhidrosis.
There are various treatments to decrease sweating, including:
- Nerve-blocking medications
- Surgery
- Botox injections
- Prescription antiperspirants or creams
Medication side effects
Certain medications or classes of drugs, including antidepressants like SSRIs and diabetes medications such metformin, can affect the activity of your sweat glands and sometimes even your body temperature.
Medication can influence sweating and affect the thermoregulatory pathway. The thermoregulatory pathway is responsible for maintaining your homeostatic body temperature. The human body stays at approximately the same temperature, or “thermoneutral zone.”
The thermoregulatory set point, or the core temperature at which sweating begins, is finely regulated and subject to the influence of centrally acting drugs. For example, serotonin syndrome or toxicity is a prevalent side effect of antidepressants like SSRIs. Studies of serotonin toxicity in humans demonstrate an increase in core temperature and increased sweating, indicating the complex action of serotonin on the thermoregulatory pathways that can be brought about by SSRI medication.
SSRIs work to treat depression by blocking the reabsorption of serotonin into neurons. SSRIs allow more serotonin to become available and thus improve the transmission of messages between neurons. But too much serotonin in the body can lead to extreme cell activity resulting in serotonin toxicity—about 10 percent of patients taking SSRIs experience episodic or night sweats.
Most cases of drug-induced night sweats may not be foreseeable. Once a drug relationship is suspected, clinical options include therapeutic dose reduction, drug substitution, or discontinuation.
Stimulants like caffeine can also be a cause of generalized sweating. Alcohol and drug use can increase the risk of night sweats. Limiting or avoiding these substances may help reduce your night sweats.
Low Testosterone
Testosterone hormone levels are crucial to normal male sexual development and functions. As men age, it is typical for their testosterone levels to drop. According to the Mayo Clinic, testosterone levels typically decline by about 1 percent annually, starting around age 30 or 40. This natural occurrence is also known as male hypogonadism, when the sex glands, or testes, produce little if any, sex hormones. Normal testosterone levels in men range from 300 to 1000 nanograms per deciliter (ng/dl). A man making testosterone less than 300 mg/dl has hypogonadism.
The common symptoms of low testosterone include:
- Low energy
- Increased body fat
- Erectile dysfunction
- Moodiness
- Hot flashes
- Low libido
If you have night sweats and other symptoms of low testosterone as described above, your night sweats may be due to low testosterone.
Low testosterone is connected to night sweats because testosterone is the primary sex hormone in men. Similar to women during menopause, low testosterone is related to hormone imbalances. Hormonal balances are relatively rare, occurring in 2 percent of men ages 50, but that sharply increases to about 50 percent of men in their 80s.